How to Manage a Tight Donor Scalp
Parsa Mohebi, MD, Jae Pak, MD, William R. Rassman, MD
NHI, Los Angeles, USA.

This lecture was presented by Dr. Parsa Mohebi at 15th annual meeting of international society of hair restoration surgery.
INTRODUCTION:
Hair transplant megasessions have pushed the amount of hair that is moved in strip harvesting, higher and higher. In the past, the focus on placing large numbers of grafts was the road block for the megasession, but as the size of these sessions has gone up progressively, the risks to donor wounds have run the gamut from wider scars, the appearance of donor effluviums; donor wound necrosis and progressively decreasing donor densities that are not always uniform. The density of hair and the laxity of the donor area are two limiting factors in perusing the larger sessions. Accurate and repeatable ways to measure the laxity of donor area can no longer be just a manual process and those doctors who are progressing to larger sessions will run into donor area

problems. We hear very little about donor area problem because they are rarely discussed. Removing too much skin increases the risk of donor complications such as wound dehiscence, necrosis and wider scars. On the other hand, decreasing the size of the donor strip makes additional surgeries unavoidable in many cases. To compound the problem, the realities of modern hair transplant drive the surgical expectations of the patient to larger session sizes for quicker results.
OBJECTIVE:
To develop a system to accurately assess the laxity of the donor area, to prevent donor wound complications and improve aesthetic results.

MATERIALS AND METHODS:
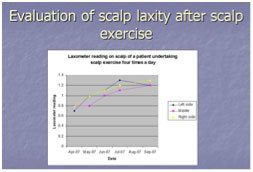
We proposed a series of steps to establish safety in harvesting a progressively larger number of grafts for new and repeat patients. Amongst the approaches, was a novel device (LAXOMETER) for establishing a metric for the mobility of the skin that could be used to assess the laxity of donor area non-invasively and a process to reduce the risks of an ever restrictive donor area. As exercises defined for the scalp may increase donor laxity in some patient, a metric was studied to show this measurement over time. We followed the use of the new metric in establishing donor wound closure by correlating measurements and scalp laxity at the end of procedure and after a course of scalp exercises.
CONCLUSION:
A reliable metric was needed for the assessment and management of scalp laxity. The authors presented the Laxometer, the tool, which will supply a metric for scalp laxity and a process for improving laxity in preparation for donor wound strip harvesting in patients with tight donor areas. The proposed process enables the surgeon to measure skin laxity non-invasively and introduces a way to improve the scalp donor laxity prior to surgery to better prepare the tight donor area for maximal harvesting. Performance of the Laxometer was presented as preoperative measuring tool for evaluation of scalp laxity and also as a intra-operative device to measure the laxity of the scalp right before excising the donor area to assure the safe width of the donor strip.